
Science
 SYSTEMS IN COLLAPSE
SYSTEMS IN COLLAPSE

ON MY Knowledge is Necessity blog, Moira commented:
"We're being told by experts to quit describing mood disorders as chemical imbalances. What metaphor or analogy shall we deploy to replace chemical imbalance?"
Moira was responding to a piece I had posted from a bipolar conference I attended in June 2009, where I had this to report: "We're not talking 'imbalance of chemicals of the brain,' Husseini Manji [formerly of the NIMH] reminded his audience. Instead, think of mood disorders as 'impairments of synaptic and neural plasticity.'"
What this means is that instead of conceptualizing the brain as some sort of uniform chemical soup that could use a bit more serotonin or dopamine, we need to see the brain as a highly intricate ecosystem that requires sophisticated nurture and cultivation. In a guest blog post, Cristina Romero had this to report from a talk by Kay Jamison of Johns Hopkins:
The brain is like a pond. It's like an ecosystem. You want to get the ideal ecosystem and then you don't want to disturb it very much. ... You want to really create a stable environment.
Allostatic Overload and Homeostasis
The brain, like an ecosystem, is highly complex, non-linear, and self-organizing. Both brain scientists and environmentalists describe this self-organizing principle as "homeostasis," where the system maintains its own equilibrium at a particular "set point." Robert Sapolsky in "Why Zebras Don't Get Ulcers" gives the example of perspiration to regulate body temperature.
But what if we're in the desert? If we keep perspiring, we will lose water and die. Here's where "allostasis" kicks in: We stop sweating buckets, our mucus dries up. Once the crisis is over, our body reverts to normal, or - in response to changing circumstances - it may find a new set point.
With "allostatic overload," we are talking system breakdown, such as what may happen with global warming or what is going on right now with the current world economic-financial situation. Allostatic overload is what happens to us when our brains fail to cope. Those of us with mental illness reach overload fairly quickly. When this happens, our brains simply don't reset to normal. We find ourselves caught in a destructive dynamic, trapped in our thoughts and emotions.
Ecosystems operate on "macro" and "micro" levels. This accounts for the "impairments of synaptic and neural plasticity" that Dr Manji was talking about. Until recent advances in brain imaging and gene technology, we had only the vaguest macro idea of neurotransmitter traffic, which gave rise to the "monoamine hypothesis" to explain mood disorders and other mental illnesses.
A gross oversimplification of this hypothesis resulted in the "chemical imbalance" myth of mental illness, best illustrated in the Zoloft ad below:
Notice how "Nerve A" and "Nerve B" are virtually empty. Here's Dr Manji's approximation of what is really going on inside the neuron:
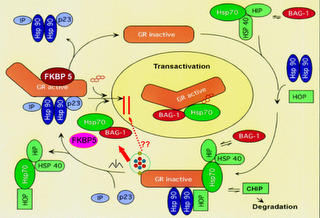
Basically, when things go wrong inside, the neuron may shrivel and even die. This connects us to the macro level.
SIGN UP FOR MY FREE EMAIL NEWSLETTER
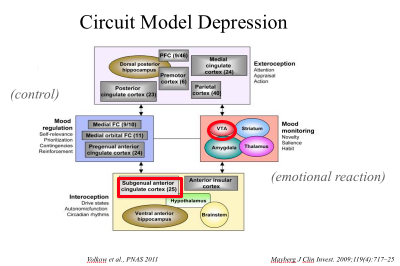
When neurons atrophy and go off-line and fail to communicate (via neurotransmitters) with other neurons, entire brain systems are compromised. We lose our ability to think and function. Here is a hypothetical diagram of the entire brain in crisis during a depressive episode (from a presentation by Nora Volkow of the National Institute on Drug Abuse):
Below is a "live view" of brain circuitry:
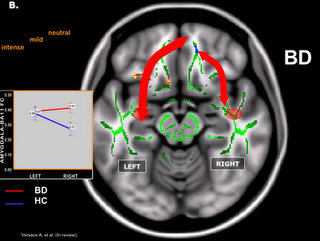
In the fMRI image (from a 2008 study by Mary Phillips of the University of Pittsburgh), we see how one particular pathway between two different areas of the brain is supposed to operate when things are going right. When things go wrong, that narrow arrow on the right becomes wide.
The arrows represent neurotransmitter traffic, busy and focused on the left, light and broken up on the right. Too much traffic on the right means the emotional part of the brain is dominating the conversation with the rational part of the brain, which happens a lot of the time to those of us with bipolar.
Macro, micro, interconnected. This is why "chemical imbalance is a myth. As Dr Sapolsky explains it, the brain is not "undifferentiated tofu." A serotonin or dopamine lube job is not going to have the same uniform result in different areas of the brain.
Macro and micro regulate the other in highly intricate. When things go right, we can only marvel at this creation of nature. When things go wrong, it's not just a chemical imbalance - it's a catastrophe, a collapse. Think "ecosystem."
Yes, But Can't We Just Find What's Wrong Inside and Fix It?
Say you come across an article (like I did), entitled "Reduced somatostatin in subgenual anterior cingulate cortex in major depression." Does this mean researchers are trying to pinpoint local brain areas as causes for particular mental illnesses? And, if so, what happens to the idea of the brain as an ecosystem?
Good question. Let's investigate, using the anterior cingulate cortex (ACC) as our model:
The ACC is part of the cingulate cortex, which snakes beneath the brain's outer cortices. The region plays a major role in modulating the two-way traffic between the brain's limbic and cortical regions. It is also wired into other circuits known as "cortico-striatal-thalamic-cortical loops," which has to do with filtering out irrelevant thoughts and emotions and sensory inputs, thus allowing us to focus on the relevant ones.
Significantly, ACC malfunction has been implicated in all manner of mental illnesses, from depression and bipolar to ADD to OCD to schizophrenia. On a most elemental level, when the brain is unable to filter out the overload, the "I" that is supposed to be in charge is overwhelmed and can't cope. For instance, in OCD the brain literally locks onto one thought and can't let it go.
In a famous set of experiments performed two or so decades ago, OCD subjects (ones obsessed with cleanliness) shared a brain scan machine with a "dirty" sweat sock. Their respective brain loops lit up like a Christmas tree. When exposed to a "clean" sock, their brains quieted down.
So - imagine (as I did in real life) someone close to you obsessed on fearful end-of-the-world thoughts, depressively ruminating to the point of psychosis or near-psychosis, and totally lacking the ability to make a rational assessment of his present and plan his future. It had to be the ACC, right?
In the aforementioned article I referred to, researchers from the University of Pittsburgh investigated whether low levels of a certain neuropeptide (somatostatin) altered ACC function (more specifically subgenual ACC function) enough to indicate a link to depression.
Yes, the researchers tentatvely concluded.
Hooray! We found the cause! Kill the fatted calf, let the feasting begin!
Interconnecting Brain Systems
Ha! If only life were so simple. In a 2008 review article in "Psychiatry," Dhwani Shah MD of the University of Pennsylvania et al point out that "psychiatric syndromes cannot be localized in a single, so-called 'abnormal' brain region." Rather, "mood and anxiety disorders involve immensely complex interconnected systems or networks of organization within the brain."
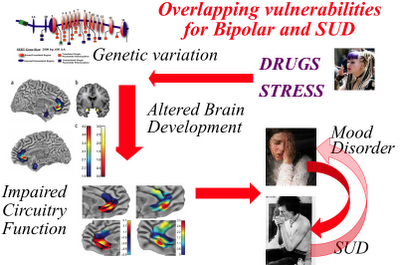
The authors are quick to point out that the causes of depression are complex and only partly understood. Nevertheless, a picture is beginning to emerge of interconnecting brain systems in a state of stress-induced collapse. In other words, a highly complex and self-regulating system failing to maintain homeostasis, as illustrated in the slide below (used by Dr Volkow to explain the stress connection in bipolar and substance abuse):
As Shah et al describe it, the brain circuitry involved in depression is grouped into three main components: cortical (appearing to give rise to the psychomotor and cognitive aspects of depression), subcortical (involving the affective aspect of depression, including anhedonia and sadness), and modulatory (regulating two-way cortical-limbic traffic, including stress and hormonal pathways).
Okay, here's where it gets interesting. Brain systems may be infinitely and infernally complex, but we are beginning to see the merit in zeroing in on specific strategic targets (or "nodes") in experimental surgical interventions. Significantly, for OCD and depression, that target is the ACC (more specifically for depression, the subgenual anterior cingulate corresponding to Brodmann area 25). This is the starting point for another article in this section on brain networks, featuring the research of Dr Volkow.
Let's be clear on this: This is not a piece extolling the virtues of psychiatric brain surgery. Indeed, it is difficult to imagine psychiatry headed in this direction. But what we are witnessing nonetheless presents us with a tantalizing peak at what tomorrow may involve. But first one more twist.
The Brain Fights Back
The homeostasis phenomenon - which occurs in all of nature - is the most credible explanation for failed long-term meds treatments, whether we are talking about the brain biologically compensating to return to where it was prior to treatment or something far more complicated, such as the destructive elements of an individual's core personality reasserting itself.
This is one reason why "what gets us well is bound to keep us well" is fundamentally flawed. Treating a brain illness cannot be equated to resetting a bone. In attempting to maintain stasis, the brain is both frustratingly and blessedly unpredictable. But in the meantime ...
Speculating About the Future
It is foreseeable that advances in technology will make MRI machines, or some other brain scan technology, convenient and affordable and routine, equating to advances in computer technology.
In the meantime, we already have the means to do gene scans - the chips are getting faster every year. Now imagine the software to interpret data coming from a whole ranges of sources - gene scans, brain scans, psychiatric evaluation, neurological testing, etc - to give the treating psychiatrist a range of options to consider.
Keep in mind, we are working off a paradigm for mental illness involving system breakdown, a host of things going wrong seemingly all at once. But suppose we could get a bit closer to the source - say the hippocampus (involved in memory) failing to boot up, say key parts of the frontal lobes going off-line, say certain stress pathways overloading. Or the ACC keeping us stuck in our destructive thoughts. Say we were able to pinpoint various signaling bottlenecks and hubs.
Thus, depression is no longer just depression. In fact, once we get a true read on what is going on, we may call its manifold variations something entirely different. All this would suggest targeted treatments and therapies, even with today's highly imperfect remedies. Perhaps a dopamine enhancer to kickstart a certain brain system rather than an SSRI. Perhaps talking therapy focusing on past trauma rather than directed at here and now challenges.
What we already know is that regulating our outside environment (such as not tempting fate in managing our personal relationships) is vital to regulating our inner environment. (See Recovery articles.)
The long-term pay-off would be that this kind of knowledge would spur future drug development (such as a med that targets somatostatin) and further refine talking therapies. It could also open the way for pinpoint treatments we can only begin to imagine.
Private investors would need to see the solid science - a clear idea of how to get from A to B to C - before they were willing to put their money on the line. The catch is this type of science is dependent on the public sector. Basic research into mental illness is notoriously underfunded as it is. For lack of will, then, we may be unable to see our way to the future, much less realize it. The Apollo program was supposed to signal the beginning of manned space exploration. We haven't been back to the moon since 1972, nor do we have the rockets for it.
The future - so near, yet so far ...
Reviewed July 11, 2016
NEW!
Follow me on the road. Check out my New Heart, New Start blog.












