
Mood
 THE BIPOLAR SPECTRUM: RECURRENCE
THE BIPOLAR SPECTRUM: RECURRENCE
Never mind the manias, for now. Simply count the depressions.
by John McManamy
THE FOLLOWING is drawn from my book, NOT JUST UP AND DOWN ...
It’s amazing how simplicity and elegance can underlie complexity and chaos. We see this in Einstein’s E=MC2, Watson and Crick’s DNA double helix, and Darwin’s theory of natural selection. With bipolar, the answer is staring us right in the face—we are looking at a cycling phenomenon.
In 1851, Jean-Pierre Falret came up with "circular insanity" and Emil Kraepelin, who coined "manic-depression," saw both depression and mania as part of the same illness, one that embraced periodic and circular insanity. The illness was “recurrent” in nature. In other words those depressions and manias kept returning. In this sense, “normal” was part of the disease process, those lucid intervals between episodes.
“Polarity” did not matter to Kraepelin. As Athanasios Koukopoulos and his co-authors point out in an editorial in the July 2013 British Journal of Psychiatry, if a patient had ten consecutive depressions, it was manic-depression. If he or she had ten consecutive manias, it was manic-depression.
Goodwin and Jamison, in their second edition of Manic-Depressive Illness, note that the modern shift to polarity discourages clinicians from thinking in terms of cyclicity and recurrence. As a result, they fail to see the illness for the episode.
Recurrence and cycling are not limited to bipolar. According to Goodwin and Jamison, these are the hallmarks of one-third or more of those with so-called unipolar depression, what they call “highly recurrent” depression. These are individuals in the course of experiencing at least their fourth depression. No manias, no hypomanias.
So, imagine being visited by your second depression in a row. Conventional psychiatry would have us disregard that first depression and not recognize the strong possibility of a third. Goodwin and Jamison and others, in effect, ask us to connect the dots, to link these supposedly separate episodes together. This is especially true when we consider that a second depression raises the likelihood of a third one occurring to 80 percent.
Essentially, people who experience recurrent depressions cycle up to “normal” rather than manic or hypomanic. In this regard, “normal” can be considered part of the disease process, an interlude between depressive episodes. This begs the obvious question: Shouldn’t this depressed population be properly regarded as bipolar? We already have a bipolar I and bipolar II. Why not a bipolar III?
This is more or less the position—with major qualifications—advanced by Hagop Akiskal and Nassir Ghaemi. Goodwin and Jamison, on the other hand, favor keeping the name recurrent depression, but stressing its kinship to bipolar.
SIGN UP FOR MY FREE EMAIL NEWSLETTER
The issue involves what Plato called “carving nature at its joints.” This gets entirely problematic if the entity in question has no joints. According to Oregon psychiatrist Jim Phelps, writing in a chapter of a collaborative academic text on bipolar II, there should be zones of rarity between two similar but distinct species.
To freely interpret, out in nature, we are not likely to come across a creature resembling a rhinopotamus. But can the same be said for mood disorders?
To understand what is going on, we need to conceptualize bipolar and a good deal of unipolar depression in terms of overlapping conditions along a continuous spectrum. Dimensions, not categories. The easiest way to grasp this is by examining the diagram below. What we are looking at is the pattern of an individual cycling in and out of depression. Note, in all three representations, the depressions are exactly the same.
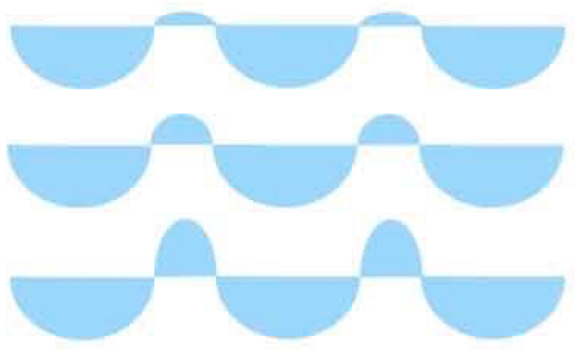
The top representation illustrates recurrent unipolar depression, separated by intervals of “normal.” The middle representation more closely resembles bipolar II, with the individual now cycling up into hypomania (mania lite). In the bottom representation, we see bipolar I in action, with the cycle topping out at mania.
Today, the DSM recognizes the bottom two representations as being related, but not the top. Instead, the DSM would have us regard the top representation as part of plain vanilla unipolar depression.
If this makes no sense to you, you are in good company. The Swiss psychiatrist Jules Angst, you will recall, is one of two men who back in the sixties coined the term unipolar depression. But he is also extremely vocal in insisting that a good many of those diagnosed with unipolar simply don’t belong there.
One of his arguments has to do with loosening the DSM criteria for hypomania. The DSM minimum time requirement is four days. But if we were to replace this with a two-day minimum, according to the Swiss psychiatrist Jules Angst, we would double or triple the bipolar population, from about two percent to five or six percent.
Minor tweak, major result. The DSM-5 mood disorders work group actually seriously considered recommending the change, but (ironically due to a newer study Dr Angst was involved in) backed off. Instead, in the back, under “Conditions for Further Study,” we have as a proposed diagnosis, “depressive episodes with short-duration hypomania.”
More germane to our discussion is the fact that hypomania is virtually impossible to recognize in a clinical setting, especially when a patient walks in the door feeling depressed. In an ongoing study of nearly 6,000 patients published in the August 2011 Archives of General Psychiatry, Dr Angst found half these individuals were misdiagnosed with unipolar depression. A more thorough exam using sophisticated screening instruments could have avoided a lot of this.
In a 2013 editorial in the International Journal of Bipolar Disorders, Dr Angst reported that 40 percent of those diagnosed with major depression are “hidden bipolar.”
Here is the problem: Try recalling how good you once felt while you are severely depressed. In this state, your brain is playing tricks on you. Memory fails you. Even raging manias—which are no-brainers to spot in real time and should be easy to recollect—fade into the dark shadows. Goodwin and Jamison, in Manic-Depressive Illness, cite a study that found that 60 percent of those showing up at their doctors depressed will deny ever having been admitted to the hospital for mania, even if the event is in their charts.
If the first psychiatrist I saw could have taken an x-ray of my life, he would have had no problem diagnosing me as bipolar I. The problem was that it never even occurred to me to tell him about how my over-the-top behavior made me unemployable twelve years earlier.
No, when something has taken over your brain—when all you can think about is throwing yourself off the balcony with a noose around your neck—you’re not looking back at all your wacky wild times. Nor do you recall the simple joys in life— the birth of your child, the thrill of nailing a tough assignment, falling in love, what food tastes like, a spectacular sunset—none of it.
This leads us to our next consideration: “Is depression a matter of bipolar waiting to happen?”
In a study published in the February 2005 Journal of Affective Disorders, Dr Angst and his colleagues tracked 406 patients with major mood disorders over a 20-year period. Of 309 patients presenting with depression, four in ten eventually manifested as bipolar—one in four of these to bipolar I, and one in six to bipolar II. Throw in those who already had bipolar at the beginning of the study and those with bipolar at the end outnumbered those with depression.
The reason no one is jumping up and down screaming from the rooftops is because these changes were gradual—like global warming—at the rate of between .5 and one percent over 12 months. So in any given year, no one was likely to parse the results of a diagnostic head-count and go, holy crap!
But holy crap!
A single snapshot of an illness, in other words, should not be taken for the real thing. Even the DSM pays some regard to this, with its arbitrary days or weeks minimum requirements. But what about the long course? Could some unipolar depressions, in fact amount to one phase in the life-cycle of the same underlying condition?
Perhaps one day, a blood draw or brain scan or genetic read-out will give us a clear and authoritative picture of what is truly going on, and so spare patients and their families years of heartbreak and frustration. In the meantime, Drs Goodwin, Ghaemi, Akiskal, and numerous others are urging clinicians to ask more questions of their depressed patients—probe for age of first onset, family history, evidence of past depressions, failures on antidepressants, and more.
They are also asking us to consider the fact that unipolar and bipolar are hardly separate species, that there is in fact a vast herd of diagnostic rhinopotami grazing in plain sight along the bipolar spectrum. Call it what you want—bipolar III, highly recurrent depression, whatever. Just don’t pretend it doesn’t exist.
Companion articles:
June 23, 2016
NEW!
Follow me on the road. Check out my New Heart, New Start blog.












