
Science
 BRAIN DEVELOPMENT
BRAIN DEVELOPMENT
Did something go wrong in childhood or adolescence?
by John McManamy
Did something go wrong in childhood or adolescence?
by John McManamy
WE KNOW that bipolar typically manifests full-blown during one’s late teens-early twenties. This is the time the brain undergoes a major neural overhaul as part of the transition from child to adult. Could it be that bipolar is a breakdown in this process?
The schizophrenia researchers have been onto this for years, and their counterparts in bipolar may be catching up. We tend to think of bipolar and schizophrenia as separate illnesses, but there is considerable overlap, particularly in pattern of onset.
There is a stage in both illnesses known as “prodromal,” which presages the main event by a number of years. There are no tell-tale symptoms, as such, merely signs of odd or worrying behavior that only appear alarming in hindsight. The schizophrenia researchers operate on the theory that the illness would be much easier to treat - indeed possibly prevent - if we could effectively intervene in the prodromal phase.
In mainstream medical thinking, with regard to physical illnesses, by the time you are noticing apparent symptoms - such your skin erupting in strange new activity - a lot of the below-the-surface cellular damage has already been done, often past the point of no-return. With regard to schizophrenia and bipolar, it is apparent that the brain is experiencing technical difficulties well before recognizable DSM symptoms appear.
The best working explanation has to do with “brain development.” I first came across this at a schizophrenia conference in 2009. In 2015, I happened upon a transcript of a 2013 talk that explained the phenomenon in a bipolar context.
Carrie Bearden is an associate professor at UCLA. In 2014, I featured her work in a piece concerning a bipolar gene study she is conducting on isolated populations in Colombia and Costa Rica. Her 2013 talk, delivered at a Brain and Behavior Research Foundation conference, dealt with risk factors in teens.
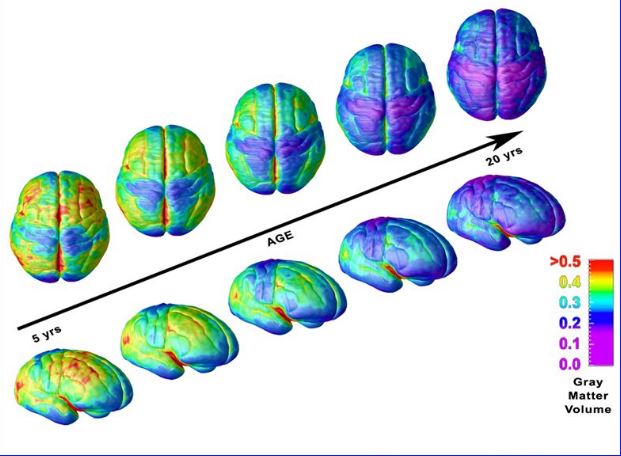
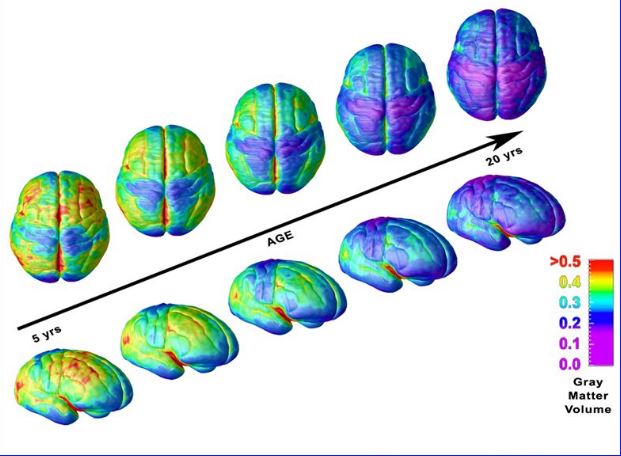
During adolescence, Dr Bearden explains, the brain loses about 40 percent of its cortical synapses. There is an actual loss of grey matter. In a child’s brain, there are excessive connections, so this synaptic (also called dendritic) pruning is normal.
In addition to grey matter changes, there are also white matter changes. White matter connects different regions of grey matter. These are basically neural axons insulated in a fatty myelin sheath. Through a process of myelination, these connections grow stronger, allowing the brain to process information and perform tasks more efficiently. The brain is myelinating up to about age 50.
The catch is that the different brain regions don’t all develop at the same time. It appears that the subcortical and limbic areas mature first, become, in effect, entirely too efficient. The cortical areas are playing catch-up, no match for the rambunctious emotional and reactive parts of the brain. Hence the phenomenon of the teen-ager.
Eventually, though, we grow out of being teen-agers. But what if, in effect, we don’t? What if something goes wrong in that critical stage of gearing up to adulthood? What if our seat of reason, in effect, proves all too easy to unseat?
SIGN UP FOR MY FREE EMAIL NEWSLETTER
According to Dr Bearden, the normal development process is disrupted in some adolescents. This is the critical period when our operating system is supposed to be upgrading our ability to regulate behavior, plan ahead, reign in impulses, and so on.
The nucleus accumbens is a region in the lower brain that is critical to the reward circuitry. During the process of development, this becomes highly activated in teens, which accounts for their risk-taking behavior. The orbitofrontal cortex, which is supposed to be regulating the nucleus accumbens, in the teen brain, is (for the most part) notoriously off-line.
Everything is supposed to even out in the end, but - wouldn’t you know it? - some of us grow up bringing barbecue to a vegan pot-luck. Doesn’t get any more risk-taking than that. At least the barbecue people tolerate some slaw on the side, but I digress.
At the same time, says Dr Bearden - during the adolescent development stage - there are circadian changes in the brain, regulated by the suprachiasmatic nucleus (SCN) located behind the eye. Dr Bearden asks us to think of the SCN as “the conductor of an orchestra,” responsible for the homeostatic process in regulating sleep and wakefulness and a host of other vital functions.
According to Dr Bearden, “we think that in people with a mood disorder, there’s something that becomes disrupted about this homeostatic process.”
Teens need plenty of sleep - typically mandating a shift to later hours - but less than 10 percent of them are getting what is considered optimal, “with adverse functional consequences.” This translates to higher risk of substance use, risk-taking behavior, depression, anxiety, and suicidal ideation.
And this is a normal population, mind you. Keep in mind - according to conventional psychiatry - an individual who has experienced depression or anxiety can return to “normal.” But someone who has been through but a single manic episode - perhaps for as short as one week - is regarded as bipolar forever.
You may have issues with this - I certainly do - but let’s at least acknowledge the gravity of the situation: On one memorable occasion at least, the rational brain has lost control, and there is a good chance it may happen again. The first manic attack, in essence, sensitizes the brain to future manic attacks.
By now, you see where this is going. Way back in the late nineteenth century, the pioneering diagnostician Emil Kraepelin - who coined the term manic-depression - observed the connection between lack of sleep and mania. The two literally fed off of each other. In those days before lithium, some of Dr Kraepelin’s patients literally died from lack of sleep.
More than a century of science has validated Dr Kraepelin. Indeed - as I have pointed out numerous times - one can easily conceptualize bipolar as a form of a sleep disorder. Dr Bearden uses the term, “sleep deviation.” The brain, in essence, has lost its capacity to regulate sleep, with devastating consequences.
There remain many more pieces to fill in, but now a picture is beginning to emerge. The picture very much parallels what researchers are uncovering about schizophrenia, though with key differences. In schizophrenia, the narrative involves the collapse of cognitive function. In bipolar, the lead story has to do with a compromise in the brain’s ability to regulate emotions and sleep.
Perhaps one day we will develop the capacity to spot the problem before it happens (say using brain scans) and administer on-the-spot fixes (your guess is as good as mine). In the meantime, Dr Bearden’s talk strongly implies that you consider this alternative universe …
Imagine a world where, back as a teen-ager, you were allowed to go to bed late and sleep in till 9 AM and not have to show up for school until 10 or 11. Would your brain have received the peace and quiet it needed to complete its long-term building project? Would your life be a lot different right now?
In the meantime, the situation is not hopeless. Check out my article on neuroplasticity.
First published as a blog in 2015, reworked into an article Jan 2, 2017.
NEW!
Follow me on the road. Check out my New Heart, New Start blog.












